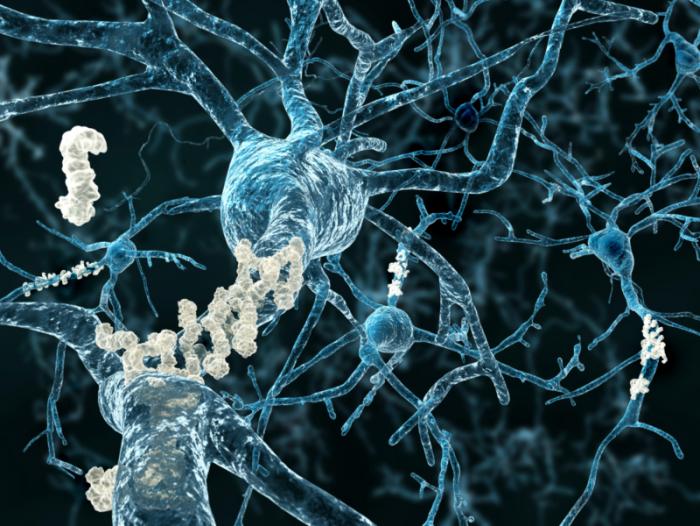
 One of the hallmarks of Alzheimer’s disease is abnormal plaques of protein fragments that build up between brain cells.
One of the hallmarks of Alzheimer’s disease is abnormal plaques of protein fragments that build up between brain cells.The study team – from Duke University in Durham, NC – report their findings in The Journal of Neuroscience.
They describe how they used a breed of Alzheimer’s mice with a more human-like immune system so they could investigate immune changes in the early stages of the disease.
The researchers found they could stop the immune cells from chewing up arginine with a small-molecule drug. When they tested it on the mice, it prevented the brain plaques and memory loss that are characteristic of Alzheimer’s disease.
They suggest their findings point not only to a new potential cause of Alzheimer’s but also to new treatment targets, as senior author Carol Colton, professor of neurology at the Duke University School of Medicine explains:
“If indeed arginine consumption is so important to the disease process, maybe we could block it and reverse the disease.”
Alzheimer’s is the most common form of dementia – it affects the part of the brain that involves thought, memory and language. Symptoms start with mild memory loss and can progress to loss of the ability to carry on a conversation and respond to the environment.
According to the Centers for Disease Control and Prevention (CDC), in 2013, as many as 5 million Americans were living with Alzheimer’s disease.
The brain of a person with Alzheimer’s gets clogged up with plaques and tangles – these are the classic hallmarks of the disease. Plaques are clumps of sticky beta-amyloid protein and tangles are twisted strands of tau protein.
Immune system changes observed in early stages of Alzheimer’s disease
The mouse model that Prof. Colton and colleagues used in the new study is slightly different to ones normally used for Alzheimer’s research. The team had developed it years before by swapping some genes to make its immune system more like that of humans.
The mouse – called CVN-AD – shows all the signs of Alzheimer’s disease: plaques, tangles, loss of neurons and behavior changes.
The team studied how the immune system of the mice changed over their lifespan. One detail they observed is that while the number of components in the immune system stayed more or less the same, within that, a type of immune cell known as microglia began to change as the mice entered the early stages of Alzheimer’s disease.
Microglia are the first responders of the immune system – as soon as there is a sign of infection, they arrive on the scene. By analyzing a molecule called CD11c that these cells brandish on their surfaces, the team found high expression of genes associated with immune suppression, and also low expression of genes that boost the immune system.
The team was surprised by these unexpected findings. Alzheimer’s researchers have been led to believe that the damage occurs because the brain releases molecules that amplify immune response.
Microglia and arginase were found to be highly expressed in memory regions
The researchers also found where neurons had died in regions of the brain important for memory, that the changed microglia and arginase, an enzyme that breaks down arginine, were highly expressed.
The researchers then ran an experiment where they used a small-molecule drug to block the arginase before the symptoms started in the mice. They found fewer altered microglia and plaques developed in the brains of the treated mice and the animals also did better on memory tests.
The small-molecule drug they used is called difluoromethylornithine (DFMO). It is being investigated in clinical trials as a human cancer treatment but it hasn’t yet been tested as a possible treatment for Alzheimer’s disease.
In this study, the team investigated the effect of DFMO on the early stages of the Alzheimer’s, before symptoms appeared in the mice. They now plan to test its effects on the disease after symptoms appear.
Findings will make us think about Alzheimer’s ‘in a completely different way’
Prof. Colton does not recommend people start consuming more arginine on the strength of these findings. Just eating more of the amino acid does not guarantee it reaches the parts of the brain that need it – and besides, the blood-brain barrier decides how much enters the brain from the bloodstream. Plus, if these findings are correct, it is the enzyme arginase that is the problem, and will continue to break down the arginine.
Prof. Colton says that the findings will point research into Alzheimer’s disease in new directions – it will make us thing about Alzheimer’s in a “completely different way,” and break the “stalemate of ideas,” as she explains:
“The field has been driven by amyloid for the past 15, 20 years and we have to look at other things because we still do not understand the mechanism of disease or how to develop effective therapeutics.”
The study was funded by the National Institutes of Health, the Alzheimer’s Association, and the Alzheimer’s Drug Discovery Foundation.
Meanwhile, Medical News Today recently learned of a study that links a diet high in methionine to increased risk of memory loss. Methionine is an amino acid found in meat, fish, eggs and dairy products.
_____________________
(Source: Medical News Today)































